Multiple Billing Types and Workflows Have You Covered
With ABELMed from one single billing screen you can bill:
- OHIP (Ontario Health Insurance Plan)
- Uninsured Services performed for the patient that they are responsible for paying
- Select Insurance Carriers providing extended insurance coverage for patients via ABELMed’s eClaim service
- Third Party’s such as companies who request uninsured services from you for their employees
- WSIB (Workplace Safety and Insurance Board)
- RMB (Reciprocal Medical Billing) for patients insured under another Canadian provincial/territorial health coverage plan, excluding Quebec
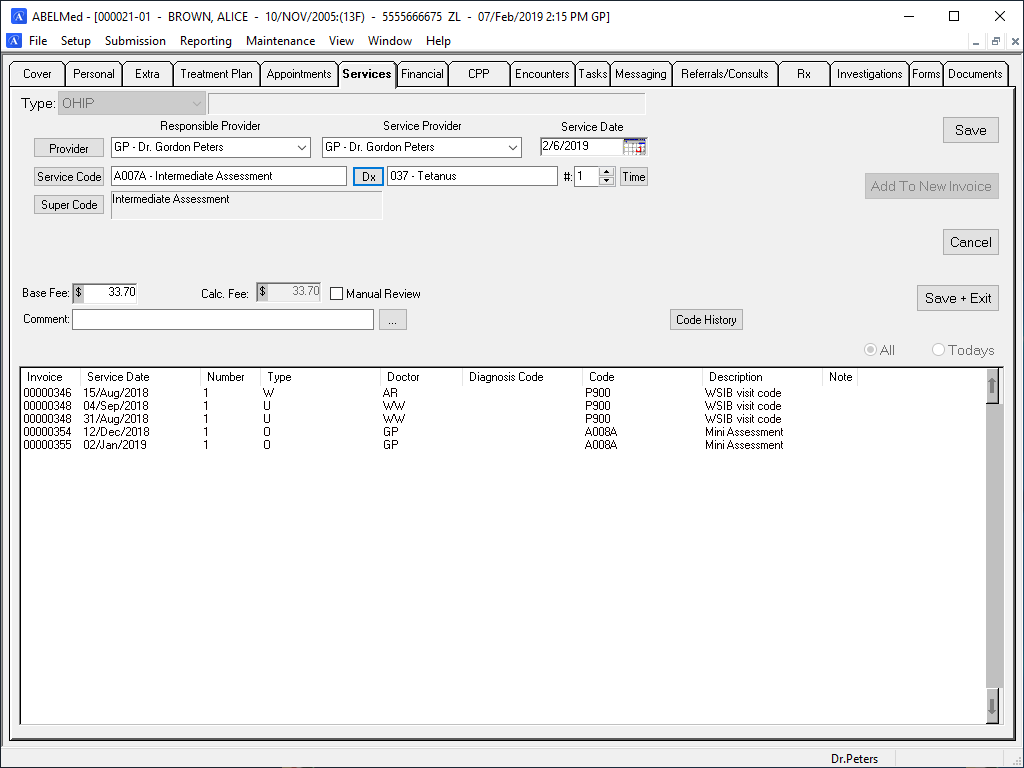
Billing Screen Time Savers
ABELMed can be setup to provide common billing defaults. For example, if billing from the scheduler, the service date, the service provider populated from the patient’s appointment details. Required but unknown Service codes and Diagnostic codes are easily searchable for quick entry. Supercodes can be created to greatly assist with common billing functions. Ie: a ‘FLU’ supercode code be setup to bill for a visit and the injection service code. A supercode can also be created to use a preset diagnosis code or providers for a single service visit. The claim is now ready for sending electronically if applicable. For direct billing, you can enter a payment and print a receipt right from the billing screen!
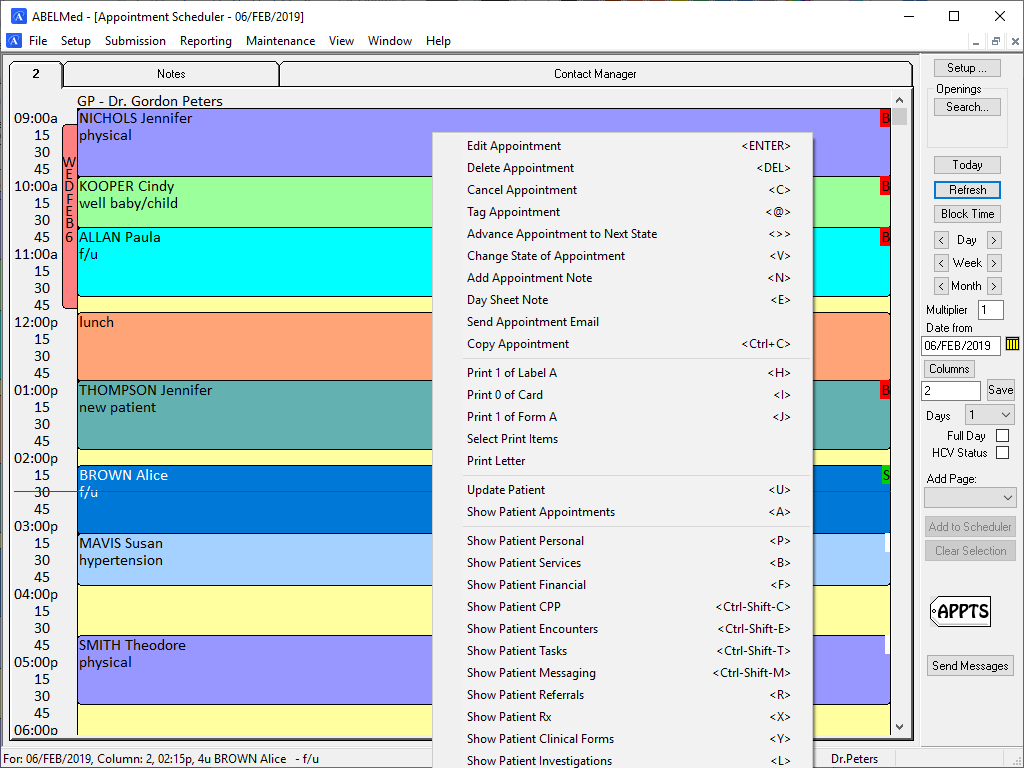
Improved Workflows – Billing directly from the Scheduler
While you can access the billing screen from the patient’s file using the Services tab, you can enjoy improved workflows by billing directly from the Appointment Scheduler. Simply move to the appointment of the patient you wish to bill for and click “B” for bill to instantly access the billing screen. Once billing is complete, the patient chart is automatically closed to return you back to the appointment scheduler. The patient’s appointment state now shown in the appointment box now changes to “B” indicating the patient has been billed.
Easy Claim Submission and Reconciliation
Sending claims, submission reconciliation, error correction and resubmission is a snap with ABELMed.
- ABELMed creates an electronic batch file of your previously created bills for submission. Simply, choose billing types, billing range, billing providers and include resubmissions if applicable.
- All your Ministry reports (Claims Errors, Batch Acknowledgment, Remittance Advice reports) will automatically be downloaded from the Ministry when you use ABEL’s convenient MCEDT Send\Receive feature. When invoices are corrected using the Claims error report, those invoices are automatically marked for resubmission so you don’t forget to include then when sending your next submission.
- After processing (any editing if necessary) the Ministry’s Remittance Advice file, the Reconciliation report is created to review the status of ALL your MOHLTC services.
Preventive/Continuing Care Reminders Using Service Codes
With ABELMed you can assign recall intervals for specific service codes. When the service code is billed, it will automatically generate a reminder (contact date for booking) based on the assigned interval. This helps ensure that required services such as annual healthcare checkups or diagnostic tests are scheduled and not forgotten.